Between August 2021 and 2023, the Centers for Disease Control recorded the prevalence of obesity at 40.3% in adults. Compulsive overeating, sometimes referred to as binge eating disorder, is a major driver of this prevalence.
Struggling with compulsive eating can feel like a lot to handle, but there are therapy options out there that work in real-world situations. Compulsive eating disorder therapy is about helping you get a grip on your eating habits, tackle emotional triggers, and develop healthier ways to cope.
What Is Compulsive Eating Disorder Therapy, and Who Can It Help?
Compulsive eating is a common eating disorder that means having repeated episodes where you eat large amounts of food even when you’re not actually hungry. It’s a loss of control usually driven more by emotions or stress than by real hunger. Unlike bulimia nervosa, there’s no pattern of purging after eating. Unlike anorexia, there’s no pattern of intentional food restriction.
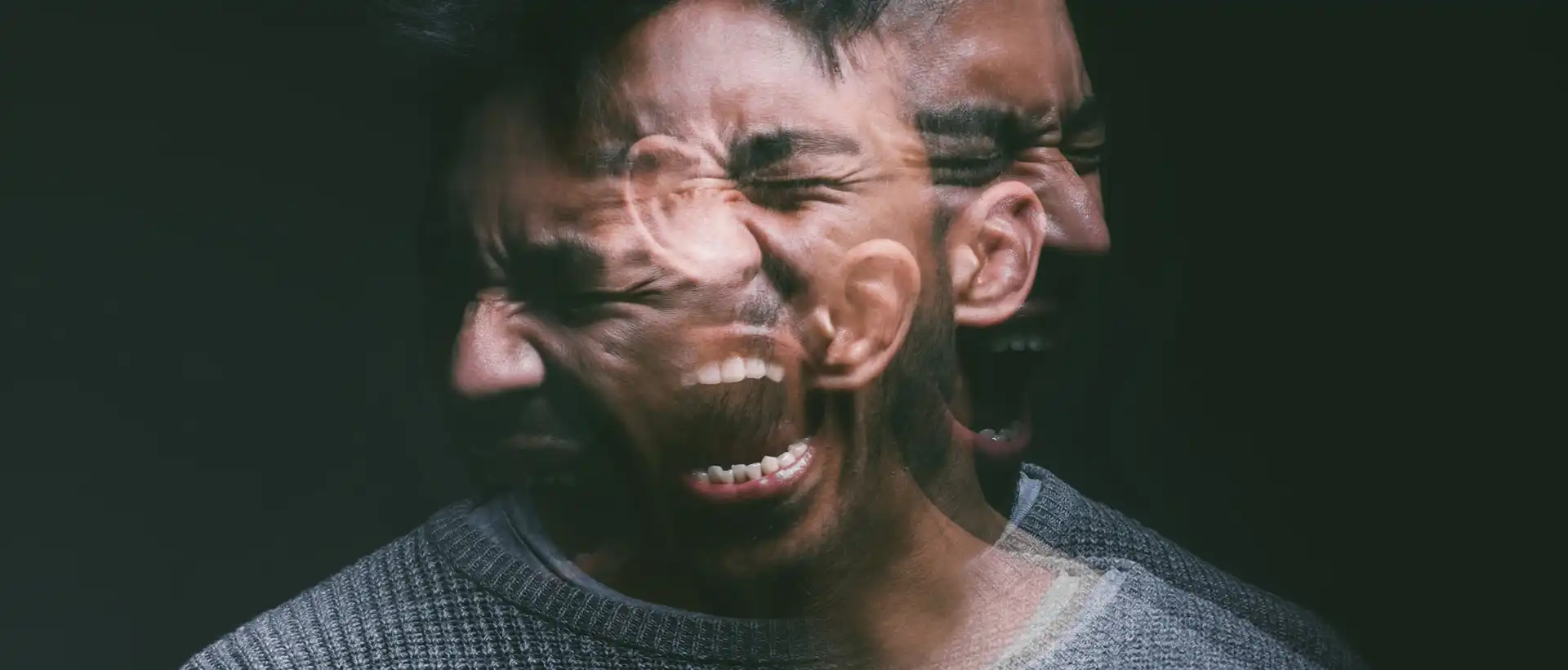
Emotional and Physical Consequences
Compulsive eating can affect both your mind and your body. Emotionally, it’s often tied to stress, anxiety, or depression. Using food as a coping mechanism might bring a short-term sense of relief, but it usually leaves you with more guilt or shame.
Physically, it can lead to weight gain, high blood pressure, diabetes, and digestive issues. You might also feel tired, have stomach pain, or trouble sleeping. If the cycle continues, these symptoms worsen.
What Does Compulsive Overeating Therapy Involve, and When Should You Start?
Treating compulsive eating disorder usually means combining structured therapy with practical skills. Identifying unhelpful thought patterns, learning to regulate emotions, and building healthier coping habits to break the cycle are the main goals of compulsive eating disorder therapy.
How Does Cognitive Behavioral Therapy Address Food and Body Thought?
Cognitive behavioral therapy (CBT) is one of the most widely used approaches for disordered eating and other mental health conditions. It helps you notice negative thinking about food, weight, and your body, and then swap those thoughts for more balanced ones.
How Can Dialectical Behavior Therapy (DBT) Reduce Emotion-Driven Eating?
Dialectical behavior therapy (DBT) is focused on managing emotions. If you find yourself eating in response to strong feelings, shame, stress, or sadness, DBT gives you tools to handle those without turning to food.
There are four main skill areas:
- Mindfulness – observing thoughts and feelings without judgment
- Distress tolerance – getting through difficult moments without self-destructive behaviors
- Emotion regulation – making emotions feel less overwhelming
- Interpersonal effectiveness – handling relationships and setting boundaries
Need Help With eating disorders?
Rehab Programs for Compulsive Eating Disorders
There are also rehab treatment options for people who need help with compulsive overeating. These eating disorder treatment programs include:
Intensive Outpatient and Day Programs
If regular therapy isn’t enough, you may consider an intensive outpatient program (IOP). These programs involve several hours a week of therapy, focusing on structured meals, coping skills, and relapse prevention.
These programs are more structured than weekly therapy but allow you to continue living at home. They’re a good fit if you need more support but not round-the-clock care.
Residential and Medical Monitoring Options
For severe cases or when outpatient compulsive eating disorder therapy isn’t enough, residential treatment might be needed. You’ll live at a facility with 24/7 support, structured meals, therapy, and skill-building in a controlled setting.
Residential or inpatient care is usually short-term. Once you’re medically stable, you’ll likely move to a lower level of care, like an OP, to keep working on recovery in a less restrictive environment.
Addressing Underlying Factors and Co-Occurring Conditions
Compulsive eating disorder is often caused by a combination of emotional, psychological, and physical factors. The best treatment plans dig into stress, trauma, body image, and any other health issues that could make recovery trickier.
Managing Stress and Emotional Triggers
Stress and tough emotions are major drivers of compulsive eating. Maybe you notice you eat when you’re anxious, lonely, or overwhelmed. That’s emotional eating, and it can be a difficult habit to break.
Learning to spot your triggers is a huge first step. Keeping a journal of your moods and eating patterns can help you see the connections.
Trauma-Informed Care
Unresolved trauma is often at the root of compulsive eating. If you’ve experienced abuse, neglect, or other painful events, food can become a way to dull or avoid tough memories. A trauma-informed approach is all about safety and trust.
Your therapist should work with you at a pace that feels manageable, making sure not to re-trigger old wounds. When trauma is addressed, the urge to eat in response to emotional pain can lose some of its grip, making long-term recovery feel more realistic.
Body Image and Self-Esteem
Negative body image and low self-esteem can fuel cycles of compulsive eating. It’s not difficult to feel stuck between strict dieting and overeating, and that often leads to guilt or shame. For some, these feelings increase the pressure to be perfect, making everything feel heavier than it needs to be.
Therapy is a place to start undoing those beliefs about weight and appearance. A weight-neutral approach shifts focus to health behaviors rather than numbers on a scale. That way, you can work on your relationship with food without tying your recovery to body mass.
Co-Occurring Mental and Physical Health Issues
Compulsive eating disorder rarely shows up alone. Many who struggle with it also experience mental health conditions like anxiety, depression, or borderline personality disorder, which can make emotional eating more difficult to manage. Addressing these together tends to work better than tackling them one at a time.
Physical health concerns may appear as well. Compulsive eating episodes can raise your risk for type 2 diabetes, heart disease, metabolic syndrome, joint pain, and sleep issues like insomnia.

Nutritional Counseling and Relapse Prevention
Treatment for binge eating disorder isn’t just about what’s on your plate; it’s about understanding how food supports your mind and body. Learning balanced eating behavior and relapse prevention skills can make compulsive overeating less likely and help you build a steadier relationship with food.
Role of Nutritional Counseling
With nutritional counseling, you get structure for making choices that meet your needs. A registered dietitian can help you set up a plan that balances nutrients, keeps your energy steady, and avoids the kind of restrictive eating that often backfires.
Accountability is a major facet of treatment; regular check-ins can help you stay on track, especially when stress or life changes pop up. It’s not just about the food itself; it’s about building habits that support recovery and make relapse less likely.
Developing Healthy Eating Patterns
Consistent eating patterns are crucial for breaking the cycle of compulsive overeating. Skipping meals or restricting food often leads to bingeing later, so keeping a steady rhythm with meals and snacks is essential.
A simple plan could be three balanced meals and two snacks each day. Each meal should have a mix of protein, complex carbs, and healthy fats to help keep your blood sugar stable and curb cravings.
Mindful and Intuitive Eating
Mindful eating is about slowing down and noticing your food. Paying attention to hunger, fullness, and taste can help you avoid eating on autopilot.
Intuitive eating builds on that foundation and teaches you to trust your body’s signals instead of following outside diet rules. You start eating when you’re hungry, stopping when you’re satisfied, and letting go of the idea that foods have a moral value.
Combining these approaches can ease the guilt that sometimes comes with eating and help you reconnect with what your body actually needs. Over time, it gets easier to step away from restrictive diets and compulsive patterns.
Strategies for Relapse Prevention
Relapse prevention is all about spotting triggers and having a plan before things spiral. Stress, feeling isolated, or being bombarded by diet culture can all make compulsive eating harder to manage.
A plan might include:
- Regular therapy sessions for ongoing support
- Meal planning to make skipped meals less likely
- Support networks such as family, friends, or peer groups
- Stress management tools like deep breathing or exercise
Fix Your Relationship with Food
Binge eating can have serious mental and physical health consequences. But there is professional help available. At Luxe Recovery, we offer compulsive eating disorder therapy to help you fix your relationship with food and take control of your diet, so you can eat what you need without letting eating itself consume you.
FAQ
What are the most effective therapeutic approaches for treating compulsive eating disorders?
Evidence-based therapies such as cognitive behavioral therapy and dialectical behavior therapy are widely used. These help you spot unhelpful thought patterns, regulate emotions, and change eating behaviors. Programs often add nutritional counseling and medical monitoring to support your overall health.
How can cognitive behavioral therapy be tailored to address compulsive eating behaviors?
CBT focuses on the link between your thoughts, feelings, and eating habits. In therapy, you’ll learn to recognize triggers, challenge negative thinking, and practice healthier coping skills. Structured meal planning and mindful eating exercises are often part of the process, helping you reconnect with hunger and fullness cues.
What role does psychotherapy play in the treatment of compulsive eating disorders?
Psychotherapy gives you space to explore the emotional and psychological drivers behind compulsive eating. One-on-one sessions can help you work through trauma, stress, or anxiety that might be fueling the behavior. It’s about treating the underlying causes, not just the symptoms.
Are there any specialized group therapy programs designed for individuals with compulsive eating disorders?
Many programs offer group therapy so you can connect with others facing similar challenges. These sessions provide peer support, reduce isolation, and help you practice new coping strategies. Some centers have groups designed specifically for compulsive and binge eating recovery.
How does family therapy contribute to the recovery process for compulsive eating disorders?
Family therapy is focused on improving communication and lowering conflict around food and body image. It helps everyone learn how to support recovery without judgment or pressure, and can address family dynamics that might be reinforcing compulsive eating patterns.
What strategies are used in therapy to prevent relapse in individuals recovering from compulsive eating disorders?
Therapists usually help you identify your triggers and figure out ways to handle stress before it gets overwhelming. They might suggest putting together a meal plan that feels doable, or encourage you to try out mindfulness.