Dialectical Behavior Therapy, or DBT, was created for people struggling with intense emotions and self-destructive habits, such as men and women with borderline personality disorder (BPD).
Over the years, it’s been adapted to help people with trauma, blending emotional regulation skills with trauma-focused strategies. A clinical study of 156 patients in a residential mental health center found that DBT therapy for PTSD showed promise in treatment.
PTSD and Complex Trauma Explained
Post-traumatic stress disorder (PTSD) can develop after a traumatic experience or even just witnessing one. Complex presentations of PTSD, on the other hand, usually come from repeated trauma, like ongoing abuse in childhood. Both can impact your emotional health, daily life, and relationships. Simply being able to recognize the symptoms and their impact is a major step.
Complex PTSD (c-PTSD) tends to appear after long-term or repeated trauma, such as childhood sexual abuse or intimate partner violence. Things like ongoing neglect, physical abuse, or being trapped in a harmful situation can lead to it. It brings extra challenges, like struggles with your sense of self, regulating emotions, and keeping relationships steady.
Both PTSD and complex PTSD affect how your brain responds to stress and threat, leaving you vigilant even when there’s no real danger. Knowing the difference can help you and your therapist choose the best treatment.
Common Symptoms and Triggers of PTSD
PTSD symptoms usually fall into a few groups:
- Intrusion: unwanted memories, flashbacks, nightmares
- Avoidance: avoiding reminders of the trauma
- Negative mood and thoughts: guilt, shame, feeling detached
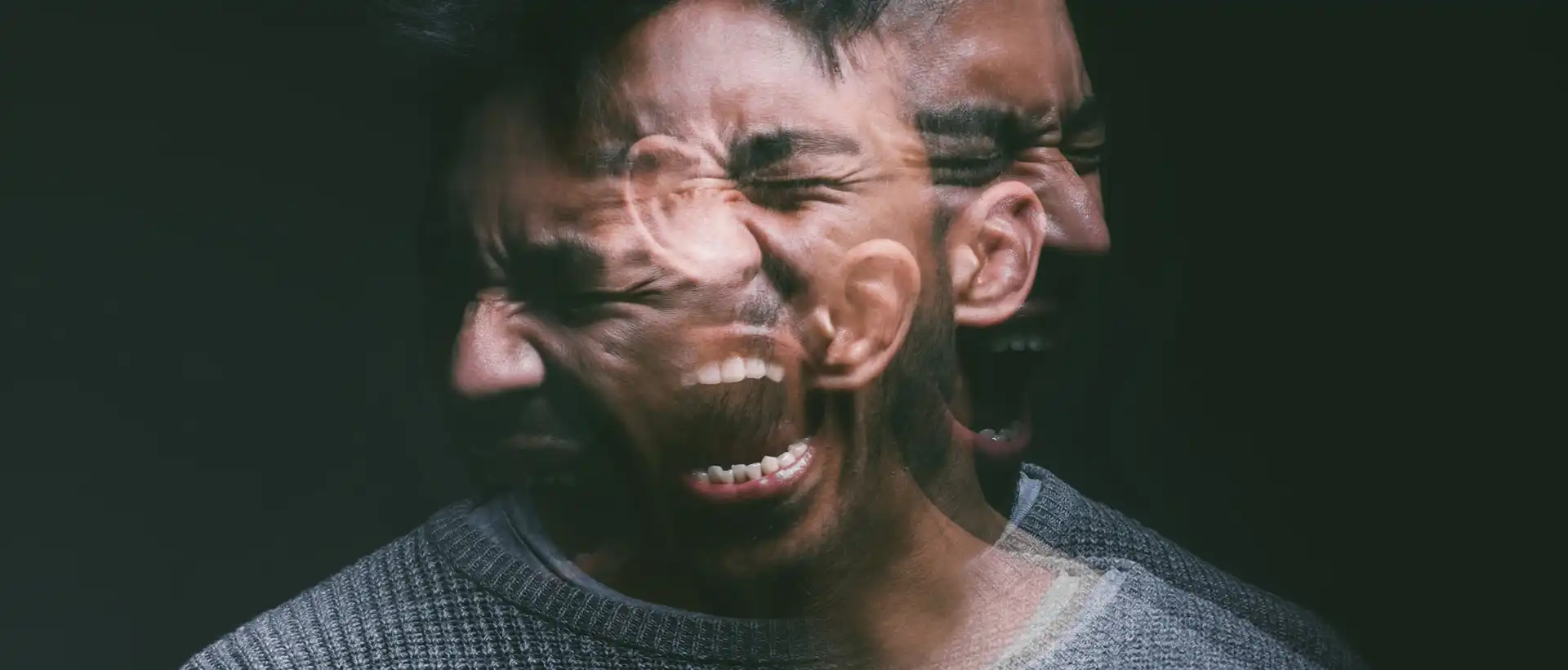
- Arousal and reactivity: hypervigilance, irritability, sleep trouble
Complex PTSD can add to symptoms like emotional numbness, trouble trusting people, and feeling worthless.
Impact of Trauma on Mental Health
Trauma can affect your sense of safety, control, and trust in others. Many people with PTSD also deal with depression, anxiety, or grief, which makes it even harder to work, keep up with friends, or feel close to loved ones.
Survivors of childhood abuse can be particularly affected because they were traumatized during crucial developmental years. This can sometimes lead to long-term struggles with self-worth and relationships.
Chronic stress from PTSD can cause sleep issues, headaches, or stomach problems. Addressing both the mental and physical fallout can help you start to find some balance again.
What Is Dialectical Behavior Therapy?
Dialectical behavior therapy (DBT) is a modality that helps you manage strong emotions, improve relationships, and reduce destructive behaviors. It mixes the ideas of cognitive behavioral therapy (CBT) with mindfulness and acceptance, aiming for real, lasting change.
Need Help With trauma?
How DBT Treatment Addresses PTSD
Dialectical behaviour therapy for posttraumatic stress disorder brings structure and a trauma-informed approach to managing PTSD symptoms. DBT treatment for PTSD is centered on reducing risky behaviors, building emotional steadiness, and creating a safer space for trauma recovery.
DBT-PTSD Model and Approach
Dialectical behavior therapy for post-traumatic stress disorder modifies the standard DBT approach to fit the needs of trauma survivors. It blends skills training with trauma therapy methods. These tools help you manage strong feelings and cut down on avoidance, which often contribute to PTSD symptoms.
Unlike some trauma therapies that go directly to exposure, DBT for PTSD takes things in stages. You learn coping strategies first, before exploring traumatic memories. This way, you’re less likely to get overwhelmed.
Phases of DBT for Trauma Survivors
DBT for PTSD usually happens in phases, moving from stabilization to trauma processing, then on to long-term recovery.
- Stabilization: You start by learning DBT basics to handle emotions, stop self-destructive patterns, and boost safety. This sets the stage for deeper trauma work.
- Trauma Processing: Once you’ve built up some stability, you start working through traumatic memories. Some therapists use the Dialectical Behavior Therapy Prolonged Exposure protocol to help you gradually face what you’ve been avoiding.
- Integration and Recovery: Here, you focus on building a life that feels worth living by strengthening relationships, chasing goals, and practicing resilience to keep from relapsing.
Therapeutic Alliance and Safety
A strong connection with your therapist is a major part of DBT therapy for PTSD. In individual therapy, you work together to build a safe space where you can face tough traumatic stress without worrying about being judged.
Safety comes first. If you’re struggling with suicidal thoughts or self-injury, DBT helps you get those under control before you start processing trauma. That way, you’re less likely to get retraumatized and can keep moving forward.
Core DBT Skills for PTSD Recovery
DBT skills can help you manage trauma symptoms by teaching you how to stay present, deal with stress without self-harm, regulate emotions, and improve your relationships. Each skill targets a different challenge that often comes with PTSD, such as intrusive memories, emotional swings, or feeling disconnected from others.
Mindfulness for Trauma Symptoms
Mindfulness is about being aware of your thoughts, feelings, and body sensations without judgment. This can reduce the immediate emotional impact of intrusive memories and flashbacks by grounding you in the present.
Simple things such as breathing exercises, body scans, or focusing on your five senses can interrupt the cycle of rumination. These skills give you a space between your triggers and your reactions.
Mindfulness also helps if you’re feeling numb or disassociated. By focusing on the present, you’re more likely to identify emotions before they overwhelm you. Over time, this can ease anxiety and depression that often accompany PTSD.
Distress Tolerance Techniques
Distress tolerance is about getting through rough moments without turning to self-harm, substance use, or other risky behavior. These tools are a boon during a crisis, when emotions may threaten to overwhelm you.
You might try self-soothing, like listening to music, holding something warm, or smelling something comforting. There’s also the TIP skill (Temperature, Intense exercise, Paced breathing), which uses physical changes to calm you down quickly.
Radical acceptance is another important part of DBT therapy for PTSD: it’s about acknowledging painful realities instead of fighting them. Practicing these skills builds resilience. You start to trust that you can get through tough times without making things worse, which is key for PTSD recovery.
Emotion Regulation Skills
Emotion regulation skills help handle strong feelings like anger, fear, or shame, all of which are common with PTSD. Instead of letting emotions take control, you learn to understand and respond to them in healthier ways.
One technique that DBT teaches is opposite action. For example, if you want to isolate when you’re feeling depressed, you might push yourself to reach out to someone instead. Acting against those impulses can help change your mood.
Checking the facts is another helpful technique. It lets you see if your emotional reaction actually fits the situation, which can cut down on unnecessary anxiety or anger. Getting better at emotion regulation lowers the risk of impulsive behaviors and makes it easier to handle day-to-day stress.
Interpersonal Effectiveness in Relationships
Interpersonal effectiveness skills help improve your relationships, especially if trauma has negatively affected them. These skills focus on clear communication, setting boundaries, and balancing your needs with others’.
The DEAR MAN skill (Describe, Express, Assert, Reinforce, Mindful, Appear confident, Negotiate) helps you ask for what you need without being confrontational. With practice, these skills can help you feel less isolated and build stronger support systems, which makes recovery more doable.

Integrating DBT with Other PTSD Treatments
When you’re using dialectical behavior therapy for trauma treatment, you might notice it works even better when combined with other approaches. Some treatments attempt to address trauma memories directly, while others focus on easing symptoms like flashbacks, nightmares, or mood swings. Combining DBT with these methods can help you manage everyday stress and get to the root of trauma at the same time.
DBT and EMDR
Eye Movement Desensitization and Reprocessing (EMDR) is a modality that is focused on helping your brain reprocess traumatic memories so they lose their impact.
If you’re dealing with intense emotions or thoughts of self-harm, DBT can lay the groundwork before you transition into EMDR. You develop tools like mindfulness and distress tolerance, which can help you stay stable enough to process trauma.
Combining DBT with Exposure Therapy
Exposure therapy pushes you to safely face memories, places, or situations tied to PTSD in controlled therapy sessions. The idea is that, over time, avoidance decreases and symptoms like flashbacks or nightmares may reduce.
DBT adds to this by giving you ways to manage the emotional fallout during exposure work. Grounding and distress tolerance skills can help you adhere to the process without getting overwhelmed.
Medication and Co-Occurring Disorders
Many people with PTSD also deal with depression, anxiety, or substance use. Medication can help ease symptoms like insomnia, panic attacks, or mood swings while you’re working through therapy.
If you’re facing multiple diagnoses, pairing DBT with medication might make it easier to adhere to treatment. A plan that combines therapy, medication, and skills practice tends to give you something solid to stand on.
There is Therapy for PTSD
Conditions like PTSD can have debilitating effects on your life. These conditions can ruin relationships, careers, and your sense of self. But there is treatment available, and some treatment approaches can be used for both conditions.
DBT therapy for PTSD can be an invaluable tool for addressing trauma. At Luxe Recovery, it is one of the many tools that we will use to personalize your treatment so you can move forward from a traumatic event.
FAQ
What are the core components of DBT therapy when treating PTSD?
You’ll focus on four main skill sets: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. These help you handle flashbacks, cut down on avoidance, and replace harmful behaviors with better ones.
How does DBT therapy differ when applied to complex PTSD as opposed to traditional PTSD?
With complex PTSD, there’s generally a history of long-term trauma and relationship struggles. DBT leans into grounding, emotional regulation, and building trust before proceeding to trauma processing. It’s a slower, safer process compared to standard PTSD treatment.
Can DBT be effectively used to address childhood trauma, and what are the specific strategies involved?
DBT can help you work through childhood trauma by teaching coping skills before you address the memories directly. Mindfulness and distress tolerance reduce the risk of being overwhelmed. Furthermore, you start identifying and shifting old survival patterns that have persisted since childhood.
What does the DBT-PTSD protocol entail, and how is it structured?
The DBT-PTSD protocol combines DBT skills with trauma-focused exposure. First, you work on stabilizing emotions and behaviors, then you gradually move into confronting traumatic memories in a structured, safe way.
What kind of training is required for therapists to administer DBT for PTSD patients?
Therapists go through specialized DBT training that covers both the basics and trauma-specific tweaks. They learn how to run skills groups, handle crises, and guide exposure work safely. Most need ongoing supervision and extra workshops to really get the hang of it.
Are there any specialized worksheets or tools used in DBT to help individuals with PTSD?
You may find yourself using worksheets to track your emotions, practice mindfulness, or try out distress tolerance skills. These tools can make it easier to carry what you learn in sessions into real life.