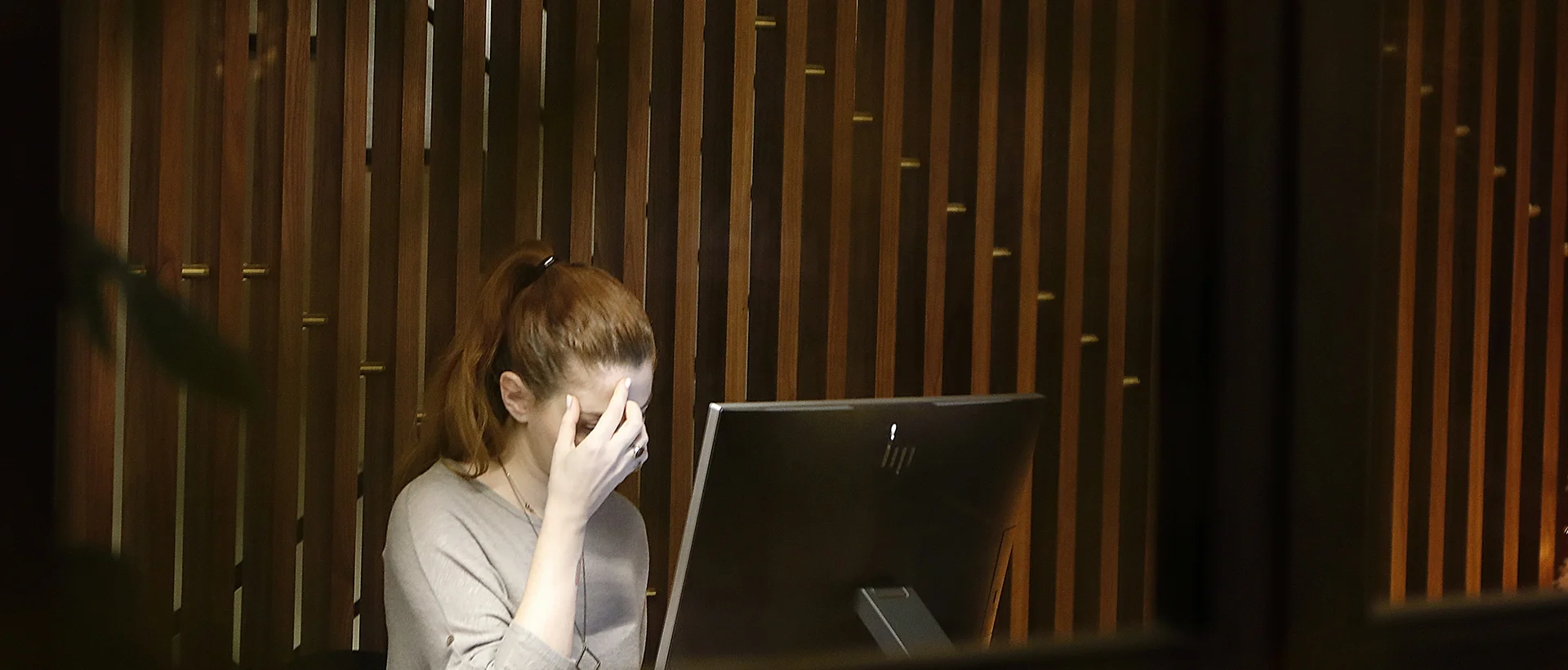
When you’re living with depression, even figuring out where to start can feel like too much. That’s why exploring the right depression treatment options matters. Remember that it’s not just about getting better, it’s about finding what works for you.
In this blog post, we’ll walk through proven depression treatment options, so you can take the next step in overcoming this condition.
Understanding Depression
Depression is a clinically recognized mood disorder characterized by persistent low mood, diminished interest in activities, and a range of cognitive and physical symptoms that impair daily functioning. It often presents with disruptions in sleep, appetite, energy levels, and concentration, and may include feelings of worthlessness or excessive guilt.
These symptoms of depression typically persist for at least two weeks and are not attributable to a temporary emotional reaction or external circumstance alone.
Understanding clinical depression requires acknowledging its multifactorial origins encompassing neurochemical imbalances, genetic predisposition, psychological vulnerabilities, and environmental stressors, rather than viewing it as a situational sadness.
Types of Depression
Depression can be classified in several distinct forms. Recognizing its type is essential in identifying the most appropriate treatment for long-term recovery.
Major Depressive Disorder
Major depression is marked by intense sadness, loss of interest, and significant functional impairment lasting at least two weeks. Individuals often experience depression with changes in sleep, appetite, and cognition.
It may occur as a single episode or recur across the lifespan, interfering with personal, social, and occupational functioning.
Persistent Depressive Disorder
Also known as dysthymia, this form of depression involves a chronic low mood lasting two years or more. Symptoms may be less severe than major depression but are longer-lasting and can significantly impair day-to-day functioning. A person may experience periods of relative improvement in mood, but symptoms rarely disappear completely.
Seasonal Affective Disorder
Seasonal affective disorder (SAD) is a subtype of depression that follows a seasonal pattern, most commonly emerging during autumn and winter months.
Research suggests it’s associated with reduced sunlight exposure and disruptions in circadian rhythm. People with SAD usually experience fatigue, hypersomnia, low energy, and weight gain that resolve as daylight increases.
Postpartum Depression
Postpartum depression is a mood disorder that can develop in the weeks or months after giving birth, which affects how a mother feels, thinks, and connects. Unlike the temporary emotional changes, these symptoms persist and often include intense sadness, emotional numbness, and difficulty bonding with the baby.
These experiences are often driven by a combination of hormonal changes, disrupted sleep, and the emotional strain of new parenthood. Because these symptoms can interfere with both maternal well-being and infant care, timely clinical support is essential for recovery.
Need Help With Depression?
Causes and Risk Factors of Depression
Studies suggest that depression is influenced by a combination of biological and genetic factors that change your brain function and emotional regulation. Specifically, neurochemical imbalances involving serotonin, dopamine, and norepinephrine are frequently associated with mood disturbances, which can affect how your brain processes reward, motivation, and stress.
Genetic predisposition also plays a key role. For instance, those who have family members who were diagnosed with depression are more likely to develop the same condition. However, it’s important to note that these biological vulnerabilities may remain dormant until triggered by stress or life changes.
In addition, psychological and environmental stressors also contribute significantly to the development of depression. Experiences such as childhood trauma, chronic stress, or unresolved grief can reduce emotional resilience and impair cognitive coping strategies over time, which can increase the risk of developing depression.
Counseling and Therapy for Depression
Counseling and psychotherapy address the psychological roots of depression by helping you process emotions, challenge distorted thinking, and develop healthier coping strategies.
Cognitive Behavioral Therapy
Cognitive Behavioral Therapy (CBT) focuses on identifying and restructuring your negative thought patterns that contribute to depression symptoms.
It helps you recognize the link between thoughts, emotions, and behaviors, and teaches practical coping skills to interrupt cycles of hopelessness or self-criticism. CBT is a structured and goal-oriented type of therapy, which makes it one of the most widely studied and effective treatments for depression.
Dialectical Behavior Therapy
Dialectical Behavior Therapy (DBT), a form of CBT, integrates emotional regulation with mindfulness-based techniques to help you manage intense mood swings.
Originally developed for individuals with borderline personality disorder (BPD), DBT has also proven effective for depression marked by emotional instability or self-harming behaviors. It combines individual therapy with skills training to promote distress tolerance and interpersonal effectiveness.
Interpersonal Therapy
Interpersonal Therapy (IPT) targets relational patterns that may contribute to or maintain your depression. It helps you understand how unresolved grief, role changes, or conflicts in personal relationships affect your mood.
By improving communication and strengthening emotional connections, IPT works to reduce depression and restore stability in your daily life. Generally, IPT offers help with depression when it’s influenced by social disconnection.

Medication Treatment for Depression
Antidepressant medications target brain chemistry to relieve symptoms that are usually used to treat depression when it is moderate to severe or persistent.
Selective Serotonin Reuptake Inhibitors
Selective Serotonin Reuptake Inhibitors (SSRIs) increase your serotonin levels in the brain by blocking its reabsorption into nerve cells. They are typically the first-line pharmacological treatment due to their efficacy and relatively mild side effect profile. SSRIs are commonly prescribed for major depression and can help improve mood, sleep, and energy levels.
Serotonin-Norepinephrine Reuptake Inhibitors
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) work by increasing both serotonin and norepinephrine, which are neurotransmitters involved in regulating your mood.
SNRIs can be chosen when your symptoms include both emotional and physical components, such as fatigue or chronic pain. Most of the time, they can be beneficial for individuals who do not respond fully to SSRIs.
Atypical Depressants
Atypical antidepressants are medications used to treat depression that work differently from standard drug classes like SSRIs or SNRIs. They may target dopamine, norepinephrine, or a combination of neurotransmitters, depending on the specific medication.
The use of atypical antidepressants is often considered when traditional antidepressants cause unwanted side effects or when a different treatment approach is needed to improve your mood and functioning.
Tricyclic Antidepressants
Tricyclic antidepressants (TCAs) are older medications that treat depression by increasing levels of serotonin and norepinephrine in your brain.
While they can be effective, TCAs are usually considered when newer antidepressants haven’t worked due to their higher risk of side effects and potential toxicity if taken in excess. Because of these risks, they require close monitoring as part of a carefully managed treatment plan.
Alternative Treatments for Depression
When traditional treatments are ineffective or difficult to tolerate, alternative approaches can help by targeting brain function in non-pharmacological ways, such as:
- Electroconvulsive Therapy: It involves brief electrical stimulation to specific brain areas under controlled anesthesia. It’s usually used for severe or treatment-resistant depression, especially when symptoms are urgent or involve psychosis.
- Light Therapy: Is a form of alternative treatment for depression that mimics natural sunlight to help regulate the mood of people with Seasonal Affective Disorder.
- Transcranial Magnetic Stimulation (TMS): uses non-invasive magnetic pulses to stimulate brain regions involved in emotion regulation. It’s typically considered when medication hasn’t worked.

What Depression Treatment Option is Right for Me?
Finding the right treatment for depression begins with understanding your overall mental health and the nature of your symptoms. Mild cases may improve with psychotherapy alone, while more persistent or severe depression usually combines therapy with medication.
In addition, co-occurring mental health conditions, previous treatment outcomes, and individual preferences also influence clinical decision-making. In cases where first-line treatments are ineffective, alternative options may be considered.
What’s important is that there’s ongoing evaluation and collaboration with a qualified mental health professional to ensure a safe and effective treatment for depression.
Your Wellness Matters at Luxe Recovery
Depression affects everyone differently, and we believe your care should reflect that. At Luxe Recovery, we take the time to understand what you’re going through, including your emotions, background, and goals.
Here, our team blends evidence-based treatments with a personalized approach to ensure that your recovery plan is tailored to your needs. With thoughtful support and clinical expertise, we’re here to help you feel seen, supported, and genuinely cared for every step of your journey.